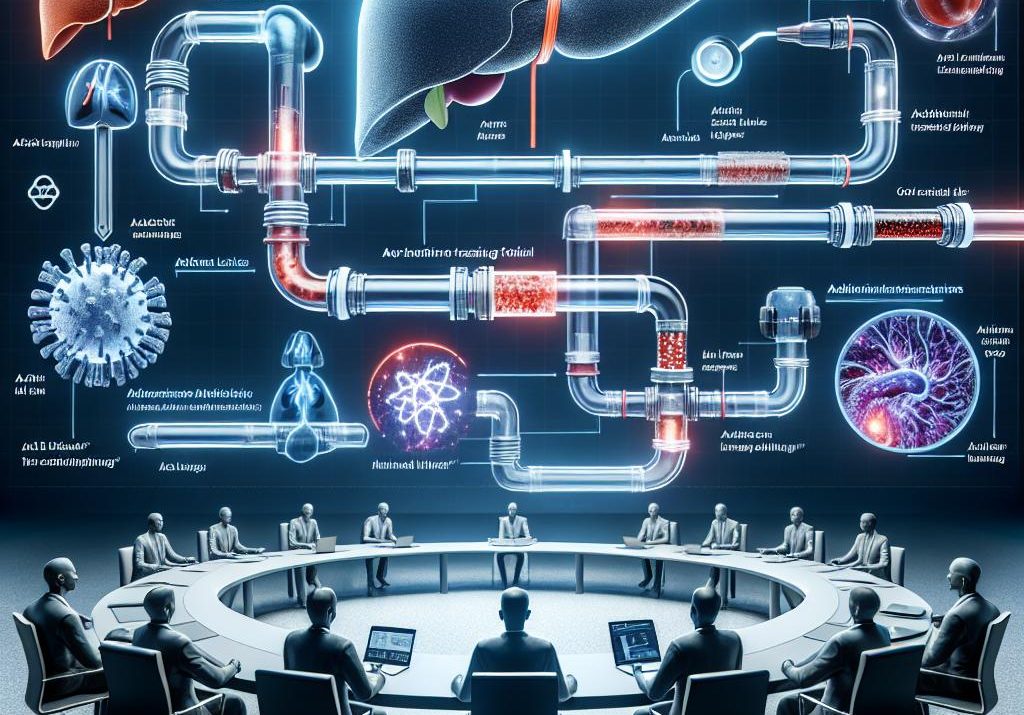
Genfit will use AASLD The Liver Meeting 2025 to showcase breadth across its hepatology portfolio, led by new preclinical and translational data in acute-on-chronic liver failure and fresh clinical updates from partner Ipsen on Iqirvo (elafibranor) in primary biliary cholangitis and primary sclerosing cholangitis. The company will present results for G1090N, a reformulation of nitazoxanide administered after an ACLF trigger, alongside two additional inflammation-targeting assets—an ASK1 inhibitor (SRT-015) and an NLRP3 inflammasome inhibitor (CLM-022)—plus real-world evidence on acute decompensation and infection-driven outcomes, patient-journey analyses in ACLF, and biomarker work in cirrhosis. Ipsen’s set of six PBC abstracts and one PSC abstract is positioned to reinforce the efficacy, tolerability, and symptom impact of elafibranor, following its 2024 approvals in PBC.
The strategy is clear: Genfit aims to own a complex, underserved inpatient syndrome with a portfolio designed to modulate systemic inflammation without compromising host defense, while simultaneously advancing a partnered rare disease franchise that is already commercial. This is an ambitious pivot from the NASH-era focus toward a hospital-first, outcomes-driven play where organ failure resolution, transplant-free survival, and readmission reduction become the currency of value. Early clinical safety and biomarker data for G1090N expected by year-end will be the near-term litmus test for whether the preclinical promise can convert into actionable clinical signals.
Why this matters now is straightforward. ACLF remains a high-mortality, high-cost condition with no approved therapies and a burden that lands squarely on hospital systems, critical care units, and transplant centers. For patients, the prospect of targeted immunomodulation post-trigger is compelling if it can reduce multiorgan dysfunction and infection-related deterioration. For payers, any therapy that shortens ICU stays, reduces renal replacement days, or lowers listing for transplant could justify premium inpatient pricing and formulary adoption. For HCPs, particularly hepatologists and intensivists navigating diagnostic delays and fragmented post-discharge care, the concurrent biomarker and RWE programs could enable faster triage, stratification, and follow-up pathways essential for both outcomes and operational flow.
Mechanistically, the slate is calibrated to current science. Repositioning an anti-infective like nitazoxanide for post-trigger systemic inflammation tackles the infection-immune dysregulation axis central to ACLF. Reviving ASK1 inhibition outside the chronic NASH setting recognizes that acute inflammatory cascades and oxidative stress may be more tractable in time-limited, hospital-managed episodes. NLRP3 inhibition reflects the industry’s growing conviction that inflammasome control can blunt downstream organ injury, with the important caveat that preserving pathogen clearance is critical in a population prone to sepsis. The discontinuation of VS-01 in ACLF, with continued work in urea cycle disorders, signals portfolio discipline and a willingness to redeploy assets where biology and development risk align.
On the chronic side, additional Iqirvo data in PBC—emphasizing both disease modification and symptom relief, such as fatigue and pruritus—continues to move payer and prescriber discussion beyond biochemical markers toward patient-centered outcomes. Emerging PSC signals, while early, sketch a path to lifecycle expansion in a disease with limited options and high unmet need, potentially reshaping competitive dynamics across rare cholestatic conditions.
The broader trend is a reshaping of hepatology after the NASH reset: targeted immunology in acute syndromes, biomarker-enabled segmentation in chronic disease, and integrated RWE to anchor hospital and payer value propositions. The near-term watchlist is tight: does G1090N deliver early clinical activity in real patients, do the ACLF RWE and biomarker programs translate into trial enrichment and operational adoption, and can Ipsen’s PSC data seed a credible expansion roadmap? The strategic question now is whether Genfit can convert a preclinical-rich ACLF narrative into a hospital-ready franchise that demonstrably trims length of stay and improves transplant-free survival—because if it can, it will not just win a category, it will define one.
Jon Napitupulu is Director of Media Relations at The Clinical Trial Vanguard. Jon, a computer data scientist, focuses on the latest clinical trial industry news and trends.